Sterilization, Disinfection, and Decontamination
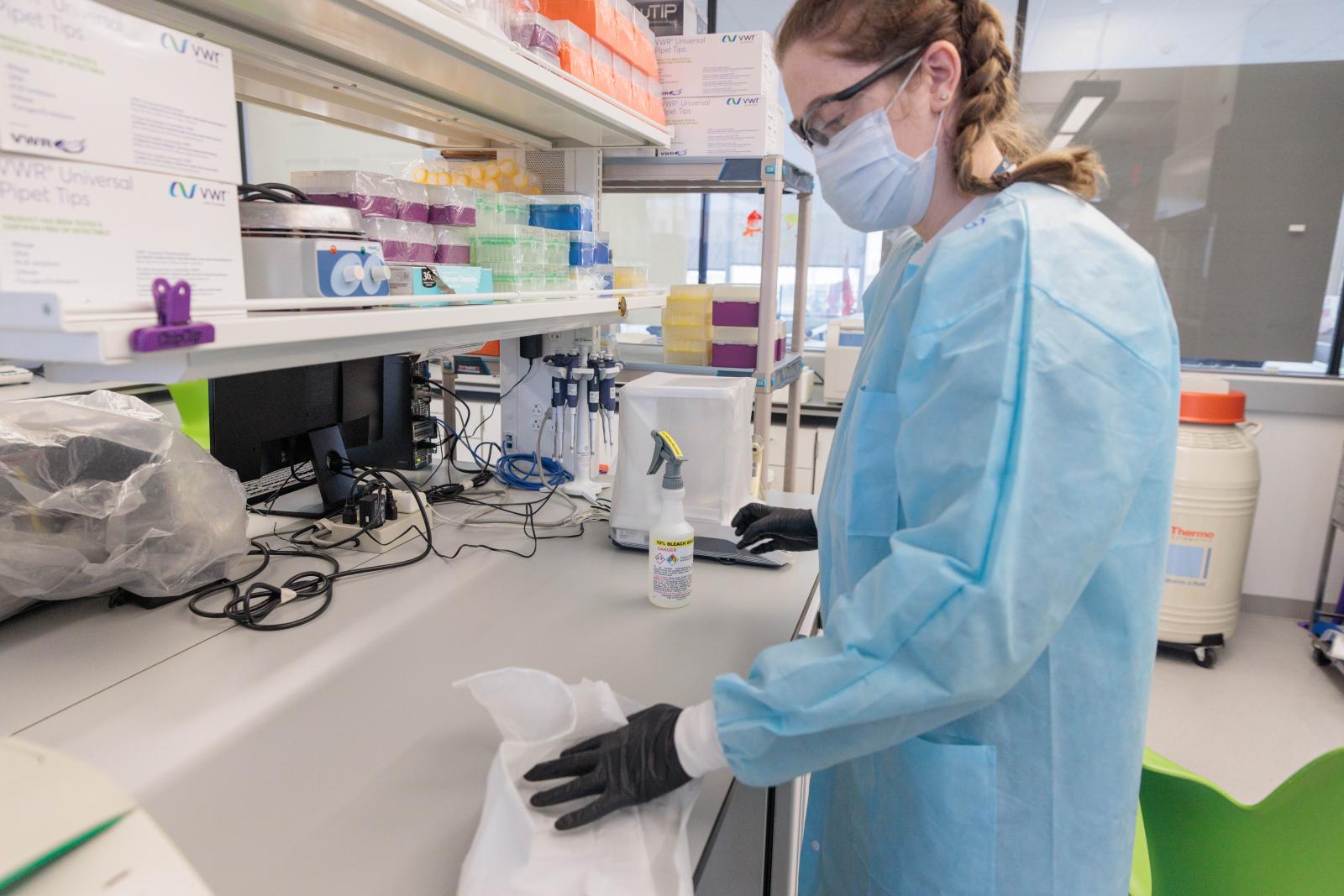
Decontamination & Cleaning
Decontamination renders an item or material safe to handle. The level of microbial contamination is reduced enough that it can be reasonably assumed free of risk of infection transmission. Sterilization, disinfection, and antisepsis are forms of decontamination.
Sterilization
A sterile surface/object is completely free of living microorganisms and viruses.
Sterilization procedures kill all microorganisms. Methods used in sterilization procedures include heat, ethylene oxide gas, hydrogen peroxide gas, plasma, ozone, and radiation.
Sterility Assurance Level - the probability of a microorganism surviving on an item subjected to treatment is less than one in one million.
Steam Sterilization (Autoclaving)
Autoclaving (saturated steam under pressure of approximately 15 psi to achieve a chamber temperature of at least 121oC for a prescribed time) rapidly achieves destruction of microorganisms, decontaminates infectious waste and sterilizes laboratory glassware, media, and reagents. For efficient heat transfer, steam must flush the air out of the autoclave chamber. Before using the autoclave, check the drain screen at the bottom of the chamber and clean it, if blocked. If the sieve is blocked with debris, a layer of air may form at the bottom of the autoclave, preventing efficient operation. Prevention of entrapment of air is critical to achieving sterility. Material to be sterilized must come in contact with steam and heat.
Chemical indicators, e.g., autoclave tape, must be used with each load placed in the autoclave. The use of autoclave tape alone is not an adequate monitor of efficacy. Autoclave sterility monitoring should be conducted on a regular basis (at least monthly) using appropriate biological indicators (B. stearothermophilus spore strips) placed at locations throughout the autoclave. The spores are more resistant to heat than most thereby providing an adequate safety margin when validating decontamination procedures. Each type of container employed should be spore tested.
Decontaminate all infectious materials and all contaminated equipment or labware before washing, storage or discard as infectious waste. Autoclaving is the preferred method. Never leave an autoclave in operation unattended (do not start a cycle prior to leaving for the evening). Log sheets should be available at each autoclave to record the name of the user, time of run, and amount being autoclaved.
All personnel using autoclaves must be adequately trained by their PI or lab manager. Never allow untrained personnel to operate an autoclave.
Disinfection
Eliminates most pathogens but not necessarily all types of microbes. Disinfection reduces the level of microbial contamination. Chemical disinfection does not kill spores, unlike chemical sterilization. Some common laboratory disinfectants include freshly prepared10% bleach and 70% ethanol.
Spaulding Classification of Disinfection
Chemical Germicide Activity Level:
- High Level Disinfection
- Comprises high concentrations of chemical germicides (ex: concentrated sodium hypochlorite).
- Kills vegetative microorganisms and inactivates viruses
- Does not kill high numbers of bacterial spores
- High level disinfectants are typically used for short time periods (10-30 min) for disinfection purposes, but may achieve sterilization if left in contact with the surface for long time periods (6-10 hours).
- Not for use on environmental surfaces like floors or lab benches
- Intermediate Level Disinfection
- Kills vegetative microorganisms, including Mycobacterium tuberculosis, all fungi, and inactivates most viruses
- EPA Approved Hospital Disinfectants which are also tuberculocidal fall into this category
- May be used for housekeeping and disinfection of laboratory benches
- Low Level Disinfection
- Kills most vegetative bacteria, some fungi, and inactivates some viruses.
- Does not kill M. tuberculosis
- Also known as “hospital disinfectants” or “sanitizers”
NB: Prions are resistant to conventional uses of heat and/or chemical germicides for the sterilization of instruments and devices. Consult Biosafety Officer for more information.
Antisepsis
Antisepsis is the application of a liquid antimicrobial chemical to skin or living tissue to inhibit or destroy microorganisms. It includes swabbing an injection site on a person or animal and hand washing with germicidal solutions.
Radiation
The Office of Research Safety discourages the use of UV lamps in biosafety cabinets.
- UV is not effective on porous materials that are opaque to the light such as wood or foam.
- UV is not effective if a microbe is protected by dust, dirt, or organic matter.
- UV light is affected by the accumulation of dust and dirt on the bulb surface.
- UV does not work in shadowed areas; penetrate into cracks or through the grill of a BSC
- Humidity adversely affects the effectiveness of UV. Above 70% relatively humidity, the germicidal effects drops off precipitously
[Burgener, J. 2006. Applied Biosafety. 11(4)228-230]